- Home
- Growth Hormone
- Growth Hormone
- Growth Hormone Deficiency
- Growth Hormone Therapy
- Growth Hormone Injections
get startedThe Most Effective Hormone Replacement TherapiesHow Stress Impacts HGH and Testosterone After 35 – What the Science Shows
Introduction
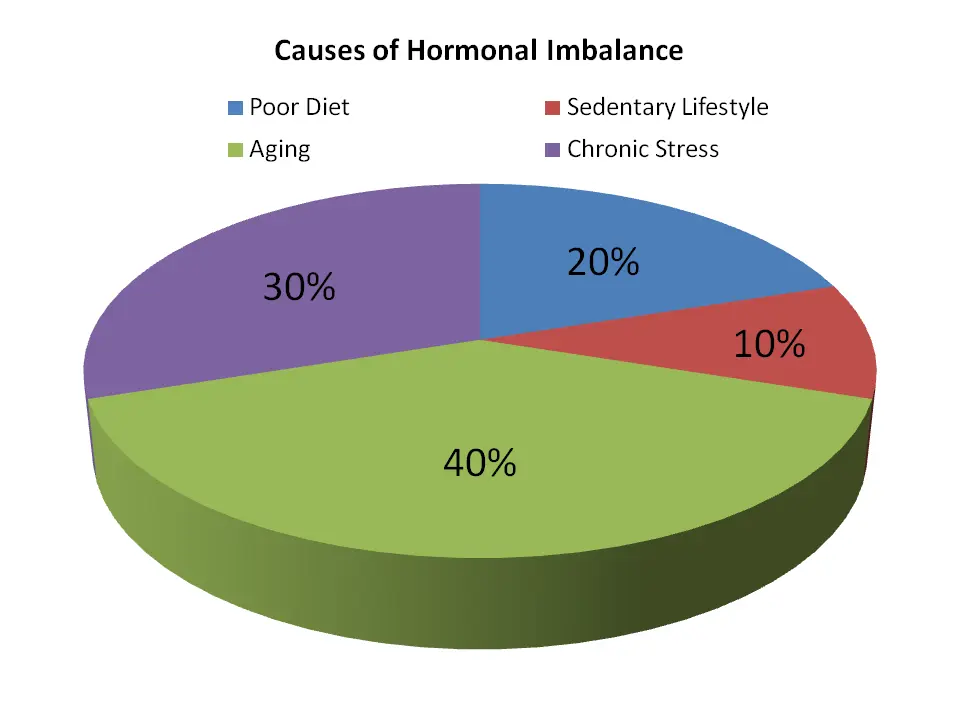
Stress has become a constant companion in modern life – especially for those juggling careers, family, and personal responsibilities in their late 30s and beyond. But did you know that prolonged or chronic stress can do more than just give you gray hairs or sleepless nights? It can also wreak havoc on your body’s hormonal balance, particularly Human Growth Hormone (HGH) and testosterone.
Both HGH and testosterone play crucial roles in energy, metabolism, muscle maintenance, mood, and sexual health. Unfortunately, many symptoms of chronic stress overlap with the signs of low HGH or low testosterone – fatigue, weight gain, irritability, and diminished libido – making it tough to know what’s truly going on without a proper evaluation**[1]**. This article presents evidence from published studies on how stress lowers hormone levels, explains why stress symptoms can mimic a hormone deficiency, and highlights the importance of blood tests for accurate diagnosis. We’ll also compare differences between men and women, discuss stress in perimenopausal women, and share strategies for reducing stress to support healthier hormone balance.
“Chronic stress can accelerate hormone decline or mimic it – leading to confusion and possible misdiagnosis.” – Dr. J. Munro, Endocrinology Researcher
Hormones 101: HGH and Testosterone in Adults Over 35
Human Growth Hormone (HGH)
- Produced by the pituitary gland, HGH supports muscle and bone strength, cell repair, and a healthy metabolism**[2]**.
- Levels are highest during adolescence and begin declining around age 30, continuing to fall throughout adulthood**[2]**.
- Lower HGH in adults can contribute to increased body fat, reduced muscle mass, slower workout recovery, and fatigue.
Testosterone
- The primary sex hormone in men, but also essential for women in smaller amounts**[3]**.
- Affects libido, mood, muscle mass, bone density, and overall energy in both sexes.
- In men, testosterone levels gradually decline – about 1% per year starting in the 30s. Women’s testosterone (from the ovaries and adrenal glands) also diminishes with age, particularly as they approach perimenopause or menopause**[4]**.
By your mid-30s, you’re producing less HGH and testosterone than in your 20s. Chronic stress can accelerate or exaggerate this natural decline, triggering symptoms that may feel far beyond “just stress.”
Chronic Stress – A Sneaky Hormone Saboteur
The Role of Cortisol
When stress hits, the body releases cortisol, adrenaline, and other hormones to activate “fight or flight.” In short bursts, this is helpful. But under chronic stress, cortisol stays elevated, which disrupts the delicate balance of other hormones:
- Lower Testosterone: High cortisol blunts signals in the hypothalamic-pituitary-gonadal (HPG) axis, resulting in reduced testosterone production in men and women**[5]**.
- Lower HGH: Chronic stress impairs growth hormone release from the pituitary gland**[6]**, reducing the body’s ability to maintain muscle mass, bone density, and healthy metabolism.
- Worsening Weight Gain: Cortisol encourages fat storage (particularly around the belly) and can break down muscle tissue over time**[7]**.
- Psychological Toll: Mood disorders like anxiety and depression can be both a cause and a result of chronic stress and hormonal imbalances**[8]**.
“Prolonged psychosocial stress is linked to suppressed growth hormone, which impairs muscle recovery and metabolism.” – Journal of Clinical Endocrinology & Metabolism
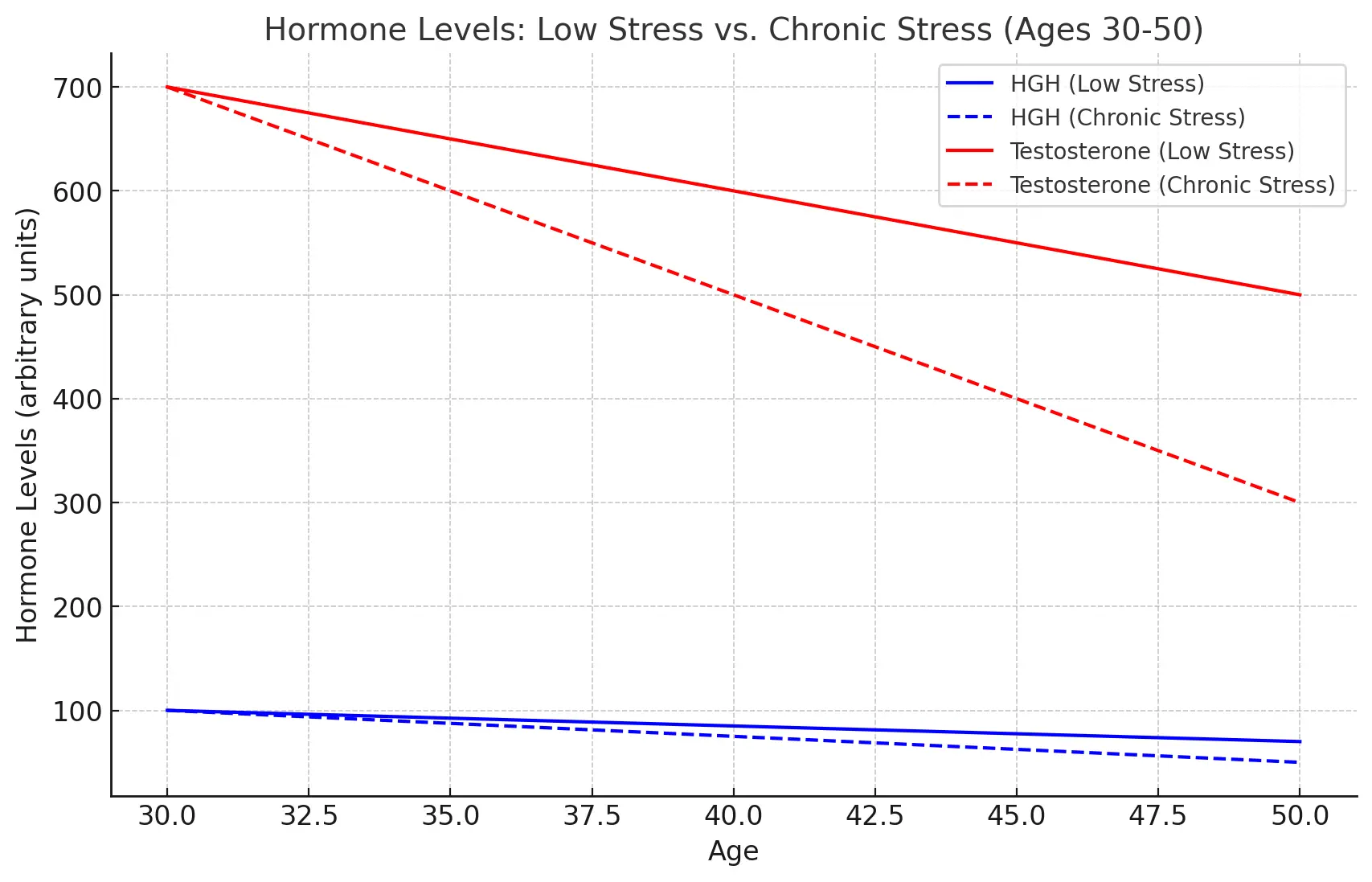
Comparison Chart: Stress vs. No Stress on Hormone Levels
To visualize the impact of chronic stress on hormone levels, let’s compare a “low-stress” scenario to a “high-stress” scenario for adults around age 35-45:
Impact of Chronic Stress on Key Hormones (Age 35+)
HormoneNormal (Low Stress)Under Chronic StressTestosterone (Men)Gradual age-related decline but usually within normal range for age (men ~300–800 ng/dL in midlife)
mayoclinic.orgLevels fall to lower-than-expected for age. Chronic stress suppresses the HPG axis, further reducing testosterone production
pubmed.ncbi.nlm.nih.govTestosterone (Women)Naturally much lower than in men (women ~8–60 ng/dL)
kingsbergmedical.comCan drop even further, since stress can disrupt ovarian function. Stress is linked to reduced gonadal steroid output
pmc.ncbi.nlm.nih.govHuman Growth Hormone (HGH)Peaks in teens/20s, then starts declining by ~age 30
med.stanford.eduReduced GH release due to prolonged stress. The body shows a “GH secretory defect” under chronic stress
pmc.ncbi.nlm.nih.govIGF-1 (Insulin-like Growth Factor-1)IGF-1 (which is stimulated by HGH) is in a normal range for age, supporting muscle and bone maintenance.Lowered as a consequence of lower HGH. Reduced IGF-1 can mean slower tissue repair and more difficulty building muscle.
lboro.ac.ukWhat the chart shows: Even without stress, adults 35+ have lower HGH and testosterone than younger adults. Add chronic stress, and those hormone levels dip even further, often into ranges that can cause noticeable symptoms. Essentially, stress accelerates or exaggerates the natural age-related hormone decline.
Key Differences: How Stress Affects Men vs. Women
Both genders experience hormonal disruption under prolonged stress, but the specific pathways and outcomes can vary. The chart below highlights some differences:
MenWomenTestosterone suppression leads to low energy, muscle loss, and libido issues.Progesterone depletion can result in irregular periods and potential estrogen dominance.HGH levels drop, slowing down metabolism and muscle recovery.Cortisol overload interferes with ovulation and overall reproductive health.Often experience weight gain linked to testosterone decline.Weight gain can occur from hormonal imbalance (estrogen/progesterone/testosterone) and metabolic shifts.Low T can trigger depression, anxiety, and low motivation.Estrogen imbalances can cause mood swings, anxiety, and more severe PMS or perimenopausal symptoms.Common Ground: Men and women both face weight gain, fatigue, and low libido under chronic stress; the difference lies in the hormonal pathways that lead to these outcomes.
Special Note: Stress and Women in Perimenopause
For women in their late 30s and early 40s, shifting hormones (estrogen, progesterone, testosterone) can magnify the impact of chronic stress:
- Estrogen Dominance: As progesterone drops, estrogen can become relatively dominant, causing intense mood swings, heavy or irregular periods, and water retention.
- Testosterone Declines Further: Chronic stress suppresses testosterone (even though levels are lower for women), exacerbating fatigue, low libido, and muscle weakness.
- Sleep Issues & Hot Flashes: High cortisol may worsen night sweats or temperature dysregulation, making perimenopausal symptoms more severe**[9]**.
If you’re a perimenopausal woman noticing unexplained mood shifts, fatigue, or sudden weight changes, evaluating both stress levels and hormone levels can be crucial.
When Stress Masquerades as Hormone Deficiency
Overlapping Symptoms
Many signs of chronic stress mirror those of declining HGH or testosterone, making it tough to self-diagnose:
- Fatigue & Low Energy: Chronic stress disrupts sleep, while low HGH/testosterone naturally leaves you tired and sluggish.
- Mood Swings & Anxiety: Elevated cortisol can lead to anxiety or irritability, just as low testosterone or estrogen imbalance can trigger mood changes.
- Reduced Libido: Both stress and low T dampen sex drive in men and women.
- Weight Gain & Muscle Loss: Stress-related cortisol elevation promotes fat storage and muscle breakdown – precisely the same pattern seen in lower HGH and testosterone**[7]**.
- Brain Fog: Difficulty concentrating could be from mental stress overload or insufficient anabolic hormone support.
“Men under continual stress often have notably lower testosterone levels, making it easy to blame stress for symptoms that may actually be a medical deficiency.” – Dr. E. Harrow, Hormone Therapy Specialist
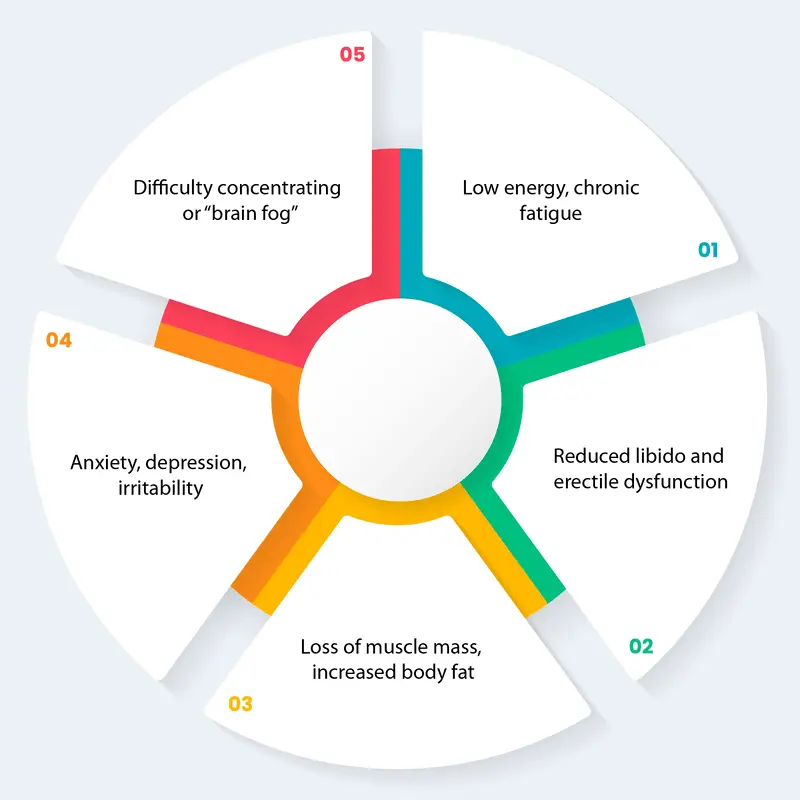
Symptoms of Stress-Related Hormonal Decline
If stress is affecting your hormones, you may experience some of these common symptoms:
For Men
- Low energy, chronic fatigue
- Reduced libido and erectile dysfunction
- Loss of muscle mass, increased body fat
- Anxiety, depression, irritability
- Difficulty concentrating or “brain fog”
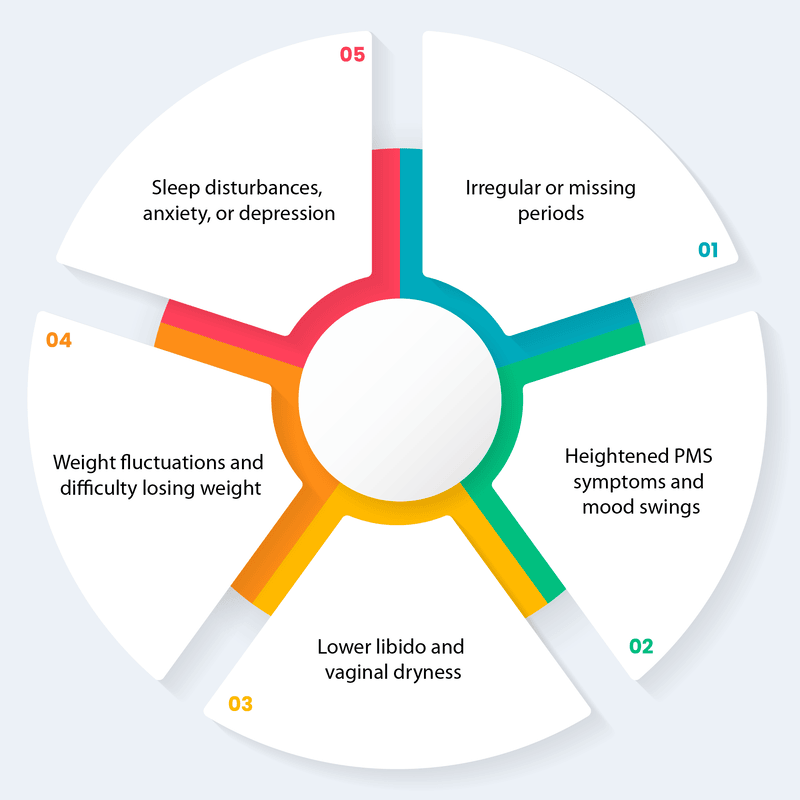
For Women
- Irregular or missing periods
- Heightened PMS symptoms and mood swings
- Lower libido and vaginal dryness
- Weight fluctuations and difficulty losing weight
- Sleep disturbances, anxiety, or depression
Note: These issues are often attributed to either “normal aging” or “stress,” but in reality, they could reflect hormonal imbalances caused or worsened by chronic cortisol elevation**[8]**.
Don’t Guess – Test: Why Blood Work Matters
Because stress symptoms can be indistinguishable from true hormone deficiency, a comprehensive blood test is the gold standard for determining what’s really going on. Typical panels measure:
- Total and Free Testosterone (for men, and sometimes for women if indicated)
- IGF-1 Levels (a stable marker of HGH production, as HGH itself fluctuates during the day)
- Cortisol and Other Markers of endocrine function
If test results show that your hormone levels (testosterone or HGH) are low for your age, a qualified medical professional can outline treatment options – ranging from lifestyle interventions (stress reduction, diet, exercise) to hormone replacement therapy, if appropriate. If your levels are normal, it’s confirmation that you can primarily focus on stress management and other health strategies without medical hormone therapy.
Remember: Without objective testing, you could be trying to address “chronic stress” when the real culprit is low T or low HGH – or vice versa.
Simple Ways to Reduce Stress and Support Healthy Hormones
- Prioritize Sleep
- Aim for 7–9 hours of quality rest. Most HGH is released during deep sleep, and testosterone also depends on good sleep**[10]**.
- Exercise Regularly (but Avoid Overtraining)
- Strength training and HIIT can raise testosterone and encourage HGH release**[11]**. Overdoing it can become another stressor, so balance is key.
- Adopt a Balanced Diet
- Include lean proteins, colorful fruits/vegetables, whole grains, and healthy fats. Too much sugar or junk food can spike cortisol and worsen weight gain**[7]**.
- Practice Mind-Body Techniques
- Yoga, meditation, breathing exercises, or even hobbies that reduce perceived stress can lower cortisol, supporting better hormone balance**[12]**.
- Consider Supplements
- Magnesium, ashwagandha, and omega-3s support stress reduction and hormone balance.
- Seek Professional Support
- If you’re feeling overwhelmed, consider counseling or therapy. Stress can be multifaceted, and talking to a specialist may help break the cycle.
Next Steps – Kingsberg Medical Referral Section
Why Test Your Hormones?
If you’re over 35 and experiencing symptoms like low energy, mood changes, declining libido, or stubborn weight gain, it may be more than “just stress.” A blood test can reveal if chronic stress is pulling your levels down or if you truly have a hormone deficiency. Either way, knowing your numbers is the essential first step.
Consult a Kingsberg Medical Professional
Kingsberg Medical offers specialized testing and personalized consultations. Here’s what to expect:
- In-depth symptom evaluation
- Comprehensive lab panels measuring your hormone levels
- Expert interpretation of results
- Tailored recommendations – ranging from lifestyle modifications to hormone replacement therapies if indicated
Call to Action:
- Fill out the contact form on our website.
- A hormone specialist will reach out, discuss your concerns, and help you schedule appropriate tests.
Don’t let chronic stress or potential hormone imbalances keep you from feeling your best. Take control of your well-being by talking to Kingsberg Medical today and start your journey toward a healthier, more vibrant life.
Important Disclaimer
This article is for informational purposes only and is not a substitute for professional medical evaluation. Always consult your physician or a qualified healthcare provider for personalized advice regarding any medical condition or treatment.
References
Below are the sources referenced ([#]) throughout the article:
- [1] The Harvard Gazette – Strong, silent, and suffering inside
- [2] National Library of Medicine – Growth Hormone Deficiency
- [3] Mayo Clinic – Testosterone in women
- [4] Cleveland Clinic – Testosterone levels and aging
- [5] Frontiers in Public Health – Chronic Stress and Endocrine Disorders
- [6] Journal of Clinical Endocrinology & Metabolism – Psychological Stress and Growth Hormone Secretion
- [7] Endotext (NCBI) – Obesity, Stress, and Cortisol
- [8] Stress and Health (Wiley Online Library) – Chronic Stress, Anxiety, and Hormonal Dysregulation
- [9] Obstetrics & Gynecology – Perimenopause and Hormonal Fluctuations
- [10] Sleep Foundation – Hormones and Sleep Quality
- [11] Sports Medicine – Effects of Resistance Training on Testosterone and HGH
- [12] Journal of Alternative and Complementary Medicine – Mindfulness Meditation and Stress Reduction
- Growth Hormone Therapy